PERSIMUNE investigates how patients with septic shock reacts to induced hypotermia
In a comprehensive study, researchers from the DNRF center PERSIMUNE, together with colleagues, have investigated whether induced hypothermia has an effect on organ failure and mortality among patients with septic shock.
Can a reduction in patients’ core temperature to 32-34 degrees Celsius (hypothermia) reduce organ dysfunction and mortality in respirator-dependent patients with septic shock? This was the hypothesis when Jens-Ulrik Jensen, a post-doc at PERSIMUNE, and post-doc Theis Itenov , carried out a comprehensive research study from November 2011 to December 2017.
They tested whether 24 hours of induced hypothermia would improve the circulation and respiratory function in patients with severe sepsis. The study was conducted in collaboration with PERSIMUNE’s head of center, Professor Jens Lundgren, along with multiple Danish and international researchers.
In the medical world, induced hypothermia – a condition in which the body temperature is less than 36 degrees Celsius – is often used during heart surgery, since the reduced oxygen demand makes possible a reduction in and complete stop of blood circulation. Concurrently, previous trials on animals indicated that 24 hours of induced hypothermia improved blood circulation and respiratory function in the test subjects.
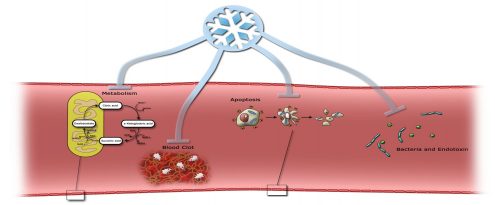
Septic shock is, among other things, characterized by severe circulatory interruptions with a higher risk of mortality than with sepsis alone. On this basis, PERSIMUNE’s research is groundbreaking because of the researchers’ investigations into how a reduction and improvement in blood circulation would have a positive effect on the mortality rate in patients with septic shock. Although this treatment option has been discussed since the middle of the previous century, it has never been researched in a big trial with an appropriate design.
The researchers screened 5695 patients from ten intensive care units in three different countries in Europe and North America and recruited 560 of them. In the randomized and controlled study, the researchers examined whether the risk of death within the first month after the patient started the trial could be reduced. Less than 1% of the patients left the trial, and the participants were aware that they were getting the experimental treatment, since the patient was physically cold.
After the 436 out of 560 patients had completed the treatment, the study was stopped because results indicated that mortality was, in fact, not reduced. Thus, the researchers had to discard the hypothesis.
However, PERSIMUNE’s groundbreaking research does not end there. The patient data collected from both this study and the team’s previous study have allowed the researchers to create a bio bank and a complete database covering most sick patients in Denmark. Further, this has allowed PERSIMUNE and other researchers on the topic to launch a comprehensive research study regarding genetics. More specifically, the study is looking at the genetics involved when two patients who apparently have similar starting points react completely differently when exposed to a very severe bacterial infection. The researchers are now able to connect this reaction with a comprehensive immunological characterization and thereby get a complete systemic biological understanding of severe bacterial infections and the host’s reaction to them.
“Within the next three to five years, we expect to be able to create the world’s first really ambitious ‘precision medicine septic shock trial,’ wherein severely ill patients are randomly receiving a treatment that is directly targeted to the specific pathophysiology that exists in the single patients, which is compared to a standard treatment. Therefore, we expect that the patients will benefit a lot more from this treatment,” said Jensen.
